
It may look like your loved one has been admitted to the hospital, but they may be there just for observation. This can profoundly change how much Medicare will pay for the stay and for any needed aftercare.


It may look like your loved one has been admitted to the hospital, but they may be there just for observation. This can profoundly change how much Medicare will pay for the stay and for any needed aftercare.

Consider strategies to emphasize quality over quantity and get rid of the obligatory activities that do not feed your soul.

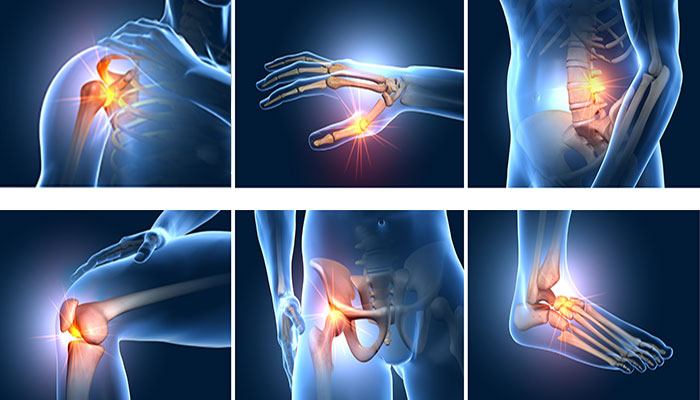
October is Bone and Joint Health Awareness Month. While disabilities often bring to mind mobility, visual, or hearing impairments, stiff or arthritic hands can be profoundly disabling. Help your loved one maintain their daily independence with these expert hacks and gadgets.

When asked about the positives of caregiving, many people report feeling proud of the ways they have grown as a person. That often involves deep vulnerability as you face new, even scary, demands. Learn tips for managing that vulnerability to your greatest benefit.

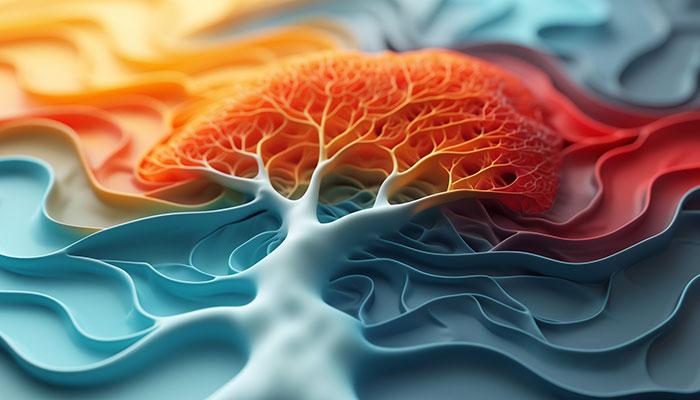
When the body is at war with itself, it’s difficult for its cells to carry on their normal, healthy processes. Fortunately, there are things you can do at home, without medications, to reduce the chance of inflammation and support a resolution to back to normal.

September is National Suicide Prevention Month. Suicide among older adults is more common than you think, especially among men over age 75 who are socially isolated and have health challenges. Be sure you know the signs and who to call if you believe that your loved one is contemplating self-harm.

Since their start in the 1980s, assisted living communities have become very popular. But the type of residents living there now is quite different from those of early years. They’re useful if they meet your loved one’s needs, but they may not be what you had in mind.

It may not be obvious, but you can usually find something to be hopeful about. So much is out of your control as a family caregiver. While hope can make caregiving easier, it’s not always easy to find. Check out these thoughts about “realistic hope” to reduce your stress and improve your own sense of well-being.

Suppose you have a car accident. Or you faint. Or get injured. Who will know to get help for your relative if something unanticipated happens to you?

Does your loved one have problems with falling but still wants to get out and get around as before? Consider a rollator. Learn about the features to look for depending on indoor or outdoor use.

Perhaps the person you care for has visual impairments. Help them retain their independence by applying these tips for navigating the world of money despite low vision.

It’s tempting to push for needed changes. But your relative is more likely to dig in their heels when you do. Resist the allure of efficiency. Instead, consider an empathetic approach with small steps. You don’t want to risk harming your relationship.

Even if you are dealing with a serious caregiving situation, taking a moment to laugh and let some humor into your life can do wonders for your own health. Laughter can help you continue on without compromising your ability to be responsible and do what is needed. In fact, it will improve your emotional stamina.

If you are concerned about your ability to safely manage all the tasks needed when your loved one is discharged from the hospital, speak up! On behalf of your relative, you have the right to appeal a discharge that seems too soon.
Joint pain, fatigue, depression, or persistent infections are just some of the possible symptoms of chronic inflammation. There is no specific blood test to zero in on the source of the problem. But the symptoms will point to the area(s) most likely affected and help the doctor investigate further.
As the saying goes, “A grief shared is half a grief.” Learn to offer comfort to a loved one without jumping in too soon with reassurances or solutions. Such responses typically backfire. While comforting for the listener, they are more likely to close your relative down emotionally.

More and more Americans are turning to complementary and alternative healers such as herbalists, chiropractors, and acupuncturists. Learn the questions to ask as you search for a provider.

Many situations in eldercare require family decision making. This is easier said than done. Learn how to arrive at a mutually agreeable solution using insights from skilled negotiators.

To honor Alzheimer’s & Brain Awareness Month, we’re looking at the link between dementia and hearing loss. The early signs of both can be quite similar, and, in fact, people with hearing loss are more likely to develop cognitive problems.

June is Elder Abuse Awareness Month. Financial abuse continues to be the most prevalent kind. Hackers, in particular, are getting very sophisticated. The latest scam is a multilayer effort to con people into transferring their savings into “protected accounts.” Warn the person you care for to be on the lookout for these fraudsters.

Patients in the hospital are rarely treated by their primary care physician. Instead, doctors who focus on the care of hospitalized patients have been found to be more effective and more available to answer questions during a hospital stay.

Sadness moves us. It nurtures compassion. It can help us feel connected with others. It can also prompt us to reevaluate our lives and make changes. Sadness is not the same as depression. It’s important to know the difference.

You might want to consider an urgent care center for non-life-threatening conditions. The wait is shorter and the stress is less than in the Emergency Room. On the other hand, the ER is more appropriate for serious conditions. How to know which to choose?

If the person you care for does not use a smartphone, with innovative new services, they can still enjoy the convenience of Lyft or Uber, no app—or hitchhiking!—required.
May is Action on Stroke Month. In that light, we look at “vascular dementia,” cognitive problems brought on suddenly by a stroke and/or gradually by “ministrokes” or “TIAs.”

Does your loved one deny there’s a problem? Resist the idea of a hearing aid? You are not alone! Learn ways to gently broach the subject.

Do you wish for the good old days when doctors made house calls? Many practitioners, including doctors, psychotherapists, physical therapists, occupational therapists, and speech pathologists, are now offering home visits (mobile outpatient services) that do not require your loved one be officially homebound.

People with conditions that limit movement, such as arthritis and Parkinson’s, often have difficulty dressing themselves. Dementia also makes dressing a challenge. Adaptive clothing enables your relative to do more for themselves, relieving you of a frustrating task and preserving their dignity and self-esteem.

When our immune system overreacts, it’s like a house on fire. This is more common as we age. Our immune system continues to tell our bodies we are being attacked, even when we aren’t, or aren’t any longer. Such “inflammaging”—the tendency in our later years to stay in an internally inflamed state—may be a common link between conditions such as cancer, diabetes, dementia, and heart disease.

While you may feel a move is urgent, the person you care for may not be ready. Don’t push! Instead, do some homework on your own so you are able to act quickly when they decide the time is right.

Between in-person and online support groups, there are many options to choose from. Make a list of your top priorities and then try out a few to see which one fits best.

If you have a disabled relative, perhaps a sibling, you may be asked to serve as the trustee for their “special needs trust.” While this is quite an honor, it’s an immense responsibility. Be sure you have the knowledge and support you will need.

March is National Kidney Month. Fully 15% of Americans have chronic kidney disease. Many are unaware of it. The condition lasts for decades, and symptoms do not appear until it is in the later stages, when irreversible damage has already been done. Should your loved one get checked?

If your loved one is having sleep problems, have them keep a sleep log for one or two weeks and then bring it to the doctor. Untreated sleep problems contribute to depression and memory loss.

These facilities are best suited to older adults who are relatively healthy. They serve as a more affordable alternative to a nursing home for those who need help only with meals, housekeeping, bathing and dressing, and getting around.

Disgust is a natural response to something distasteful. But it can be distressing when it arises in the course of your caregiving duties. You may not be able to get rid of it completely, but there are things you can do to reduce the intensity.

If you’re worried about dementia, it may be that memory or thinking problems are being caused by conditions that can be treated and reversed. Remove the anxiety by getting a full medical evaluation.

If your older relatives did not learn Internet skills during their work lives, you may be getting calls to provide tech support. It can be frustrating, inconvenient, and perhaps not even the best for your relationship. There are alternatives.

February 4–10 is National Burn Awareness Week, a good reminder to review precautions that can protect your loved one from harm.

If your partner has received a dementia diagnosis and is still working, consider these resources to help address the impact it will have on your family finances.

If you feel guilty and have regrets as a family caregiver, you are not alone. It could be because you are overstressed. Still, regret can be a useful signal that it’s time to do some thoughtful reflection and decide on future actions.

Learn tips to safely and effectively assist your visually impaired loved one, especially if they are in unfamiliar territory.

The skin is the body’s largest organ and its essential “armor.” To maintain good health, skin needs extra attention as we age. The skin has three layers. Working together, they act as the body’s shield by preventing bacteria and viruses from getting into the body and keeping body fluids from evaporating out; insulation by preserving…

Help the daily caregivers develop a fondness for your relative and view them as more than “the hip replacement in 210.” Showing a genuine interest in the life and daily experience of the aides will go a long way toward building a congenial sense of teamwork.

While many older adults do just fine with a regular consumer-grade tablet, others do better with a “senior tablet,” which has safety precautions and a simplified interface. Learn what to look for if you are considering one for your relative.

Providing comfort and calm is the watchword for the day of travel with a person who has dementia. Take advantage of the help that is available from airport personnel.

Failure to follow medical advice is one of the primary reasons older adults end up in the hospital. What can you do to help your loved one adhere to the doctor’s orders?

If your loved one has COPD, it’s important to understand which foods are most helpful and which should be limited. You might be surprised by the difference nutrition can make!

As a family caregiver, it’s easy to put your own needs last. You may feel it is a virtue, but actually, you are putting yourself and your loved one at risk. You simply have to take breaks and to safeguard your own well-being. Caregivers who don’t experience significant mental and physical health consequences.

How to pay for care is a big worry for families. Learn about options for financial support, as well as tax and workplace protections to assist you as the family caregiver. There are also legal documents your loved one will need to prepare to be sure their wishes are followed. For that, it’s best to work with an attorney.

November is National Family Caregivers Month. Whether you are new to family caregiving or have been doing it for a while, we outline the top strategies that will help you navigate the process effectively and keep stress to a minimum. This week we focus on gathering information and finding help.

November is COPD Awareness Month (chronic obstructive pulmonary disease). If your loved one has respiratory problems and needs oxygen, they can still travel by plane. You just need to plan ahead.

Perfectionism is a mental habit that can get in your way as a family caregiver. Your intentions are the best, for everyone. But it will be better for you, and your loved one and family, if you can develop a more nuanced approach where doing the best you can REASONABLY do is the gold standard.

Many families instinctively feel that the amount of money spent on a funeral reflects the love felt for their departed relative. Not so! That belief can result in unnecessary debt. Consider separating the disposal of the body from the memorial service and focus on what will be the most personally meaningful for survivors.

Pain is no fun, whether in a knee, a neck, or elsewhere in the body. There are drugs that dull pain. But they don’t cure the problem. Plus, prescription drugs usually have side effects or are addictive. Physical therapy (PT) is a proven treatment that can relieve pain and in some instances, cure the problem.

Perhaps you wonder if your family member is a “hoarder.” (You may even harbor secret fears about yourself!) We all have cherished possessions. From trophies to teacups. Spare buttons to cans of half-used paint. But hoarding is different.

Does your loved one need to downsize? Move? Does the prospect seem overwhelming? Perhaps not just physically, but emotionally too? Enter the senior move manager: Part mover, part interior decorator, part compassionate friend. These professionals take a holistic approach. They handle the physical logistics. They are also skilled at assisting older adults with the emotional side of a move.

This is World FTD Awareness Week. People with FTD often exhibit sudden changes in behavior or personality. FTD is frequently misdiagnosed as Alzheimer’s disease, depression, or some psychiatric disorder. It is the most common form of dementia for people under 65 (early-onset dementia).

National Stepfamily Day falls in September. To honor these special families, we are featuring an article about working with stepsiblings. It could be that you have hardly met your “brothers and sisters,” yet you may be called upon to work together in an eldercare crisis.

September is Pain Awareness Month. Consider addressing your loved one’s pain with tips from music therapy. No drugs. No side effects. Simply drawing on the mind-body connection to lift mood, enhance relaxation, and distract from pain.

A difficult or abusive childhood makes for a very uncomfortable caregiving situation when your parent begins to need help in their later years. You don’t have to do it all. Consider these strategies for doing what feels right while also taking care of yourself.

Support your loved one’s independence with simple but important low-vision adaptations in the bathroom: Color contrasts, a magnifying mirror, a shower caddy, etc.

The U.S. Surgeon General reports we have a loneliness epidemic. Like smoking and obesity, social isolation creates a greater risk for poor health. It’s been associated with a 48 percent increase in “premature death” (a death where a change in lifestyle could have resulted in a longer life). Our social health affects our physical health.

It will likely take one to three months for you and your loved one to get used to the new living situation at memory care. Strong emotions are to be expected. But there are strategies to ease the transition and promote a resilient recovery for both of you.

Have you spent years encouraging a loved one to steer clear of salt or avoid fat? There is no doubt that a healthy diet can promote longevity. But there does come a time when quality of life is more important.

Is being selfish always bad? Is it possible to be too altruistic? Take the survey to see where you stand. It could be that you and your loved one would benefit from your being a little more selfish—in a healthy way.

Once you’ve decided to go, there are a few things you can do weeks ahead of time, and then while packing, that will ease many of the challenges that might arise in the course of your travels.

If your loved one is frail or has dementia but needs treatment for pneumonia, a urinary tract infection, or a flare of heart failure or COPD, you may be eligible for a Hospital at Home program. A team of professionals mobilizes to treat your relative at home. Popular in Europe, this program provides quicker recovery without the common setbacks of a hospitalization.

For Elder Abuse Awareness Month, we look at the problem of bullying and exclusion in senior housing. It’s surprisingly common. Fortunately, there are things you can do, whether your loved one is on the receiving end or the “bully” themselves.

A relative’s serious illness pushes us to communicate deep thoughts and bring closure to the relationship before we lose the chance. Don’t postpone those discussions! They may be awkward, but they can be profoundly important for all involved.
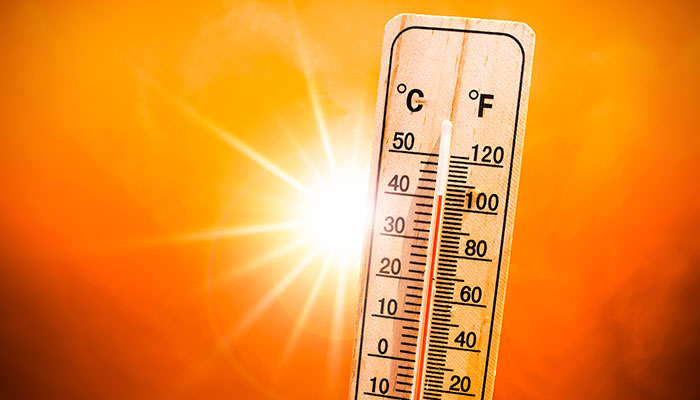
Extreme temperatures are especially hard on older adults. There are things you can do for your loved one to reduce the impact of a heat wave this summer, even if you live far away.

Are you hoping to travel this summer with a loved one who has dementia? New and crowded situations are notorious for creating confusion and outbursts. Take a moment to reflect on your relative’s likely reactions and what you can do to keep them comfortable.

June 15 is World Elder Abuse Awareness Day. There are seven different ways that elders can be exploited. Learn what they are and how to report it if you suspect a problem.

As a family caregiver, you need to take a break now and then. It’s not selfish. It’s essential! But in order to truly rest, you’ll want to be sure your relative is covered.

National Cancer Survivors Day is coming up (June 4), which celebrates the fact that 66% of those ever diagnosed with cancer are still alive five years later. Help your loved one get a jump on any potential cancer by taking advantage of these free screening tests.

Nearly one in four older adults experiences ringing in the ears, called “tinnitus.” For some, it interferes with concentration and is so severe it leads to insomnia, depression, and anxiety. In honor of Better Hearing and Speech Month, we highlight what you can do to help your loved one address this all-too-common condition.

Once you decide memory care is the wisest path, the next step is choosing a facility and creating a smooth moving day. Many memory care communities have a “move-in coordinator” or other family liaison. Rely on this professional for guidance.

A long-time hospice nurse—someone deeply committed to caring for the seriously ill—created this list of the top five deathbed regrets she frequently observed in her patients. She vowed to take these lessons to heart. Do any of these ring true for you?
If your loved one is admitted to a skilled nursing facility, Medicare requires the staff develop an initial, personalized care plan within the first 48 hours. This describes who should be doing what. Then, within the first 14 days, the staff must assemble a comprehensive assessment, which must include your loved one’s needs and strengths.
It’s important to do the best you can when caring for a loved one. But aiming for perfection can bring on problems. For yourself, in terms of anxiety, depression, and low self-esteem. And for your relative and other family members, who may feel burdened by living under the stress of constant measurement and judgment.
For many people, a pillbox is just the ticket. But as we age, we may take more medicines. Filling the box requires more concentration. Remembering to take the meds can become more challenging. Many families turn to technology to help an aging loved one.
If you are the person most likely to step in if your loved one is unable to get to the bills—a hospitalization, dementia—you need to get oriented. And organized! It’s easy to lose track of paperwork, especially someone else’s. Professionals recommend gathering important documents in a file or binder for safekeeping. Put that in a locked and fireproof location. Consider a small home safe. Or a safe deposit box at the bank.

April 10 is Siblings Day! How are things going with your siblings? Does everyone in your family participate in the care of your loved one? Is there agreement on the problems? The solutions? If not, you aren’t alone with this issue. But you could probably use a family meeting or two to get everyone rowing in the same direction.
If your spouse is younger than 65 and has received an Alzheimer’s diagnosis, you may feel in a world all your own. You probably don’t know anyone else in this situation and may sense a social stigma. It can be scary. Lonely. And feel just not fair!

Did you know “false teeth” need to be brushed daily, just like “real teeth” do? Learn how you can help your loved one avoid infections, maintain good nutrition, and extend the life of their dentures.

Food is so profoundly linked to health and love, it can be distressing to realize that someone you care for is missing meals or otherwise eating poorly. There are many services available to help, each with their own special procedures. Learn about the questions you’ll want to ask.

People with moderate dementia are rarely aware of their need for help. It will be the family members who make any placement decisions. How do you know when this option should be explored?

If someone else in your family has primary responsibility for the care of your loved one, that doesn’t mean you don’t have anything to contribute. Far from it! Caring for an older adult is more than one person can do alone. There are many ways to lend a hand (even if you don’t live nearby).

February is Heart Month. If your loved one needs frequent naps and gets out of breath easily, he or she may need a daily life energy budget. (This is especially true for people with heart failure.)

If the person you care for has a low vision diagnosis, three types of modifications to the home can make life easier: Lighting, glare control, and the use of color contrast. Fortunately, these strategies are relatively inexpensive.

Frustrated in your search for a paid caregiver? You are not alone. There is an extreme shortage of helpers right now. Even before COVID, the demand for aides was greater than the supply. The “Great Resignation” hit the caring professions hard. Caregivers close to retirement left early. And many younger workers decided to opt for safer, less demanding jobs. In some states, as many as 38% of direct-care workers chose other occupations last year.

Caring for a parent long distance brings its own challenges. With planning, organization, and frequent communication—plus a little help from technology—you can provide effective support.

Catching things early is big with Medicare. Every year, all Medicare enrollees are eligible for a free “Wellness Visit” with their primary care doctor. This is NOT an annual physical, so don’t use that term when making the appointment. Beyond basic vitals—height, weight, blood pressure, and pulse—there is no physical examination. If a physical exam is done, your loved one may have to foot the bill.

Being primary can be quite a job. In many cases it involves driving to the doctor and managing medications, handling finances, providing for daily needs, coordinating care services, and keeping the elder’s spirits up. If you are that person, don’t try to do it alone—even if it seems like that’s the only choice.

Our eyes show us the world. If something goes wrong with them, it can affect our total well-being. Dry eye syndrome makes eyes feel gritty, burning, itchy, and sensitive—discomforts that are hard to ignore! It typically manifests with age and affects as many as 30% of older adults.

The dangers of cold weather are obvious outdoors. But there are dangers indoors, too, most often because the house thermostat is set too low. People can die from being too cold. Older adults are especially at risk.

Take any roomful of people and likely two-thirds of them have relatives who aren’t talking to each other. Families are messy. Hurts abound. Some people wait until a serious diagnosis to reconcile. They often regret the years of separation they can never retrieve. Others try forgiveness earlier in the process. There’s no right or wrong.

The grandparent–grandchild relationship can be precious, like no other. But even young children notice if Grandma or Grandpa isn’t acting the way they used to, or the same way others do. And they will have questions.

If you expect older visitors this season, check your home for hazards. Older adults often have impaired balance and vision. This makes them prone to falling, especially in new surroundings. And fragile skin and bones can mean double trouble if someone does take a spill.

Taking the right medicines at the right time is extremely important to health management. But 75%–96% of older adults admit that they frequently make mistakes with their medication. Is your loved one among them?

Deciding what holiday gifts to give a person with memory loss can be challenging. From seasonal activities to digital picture frames or fuzzy robo-pets, we’ve got suggestions!

November is National Family Caregivers Month. We want to express our gratitude to you, who are part of the 40 million people (one in six Americans) who care for an older adult friend or relative. So many family caregivers feel invisible, we thought we’d give you some perspective on the scope of family caregiving across the country.

Are frequent visits to the ER a significant part of the past six to twelve months? Does your loved one seem more fatigued? Less interested in eating? Perhaps a bit withdrawn? These symptoms may be hallmarks of a serious illness your relative will overcome. But it’s also possible that these signal that your family member no longer has the reserves to beat their condition.

If the person you care for is a veteran and is seriously ill, they may qualify for a VA program designed to control symptoms that cause pain, discomfort, or mental or emotional distress. Called “palliative care,” this program is available even if the problems are as a result of treatments, not just the medical condition itself.

Do you ever wish you could wave a magic wand for more joy? Patience? Optimism? Motivation? Maybe less irritability and stress? It’s actually accessible now, no wizardry required. Just a shift in attention. Welcome to “anticipation.”

The most common form of dementia is Alzheimer’s disease. However, there are many other conditions that also bring on memory problems. It is important to accurately identify the cause, even if there’s no cure, because this will shape the best strategy for addressing difficult symptoms.

It’s unpleasant to imagine that your loved one might become the victim of crime, but it’s worth considering. There are valuable preventive steps to take. Unless your relative lives in a high-crime neighborhood, their greatest risk is a property crime in or around their home.

If your loved one is discharged from the hospital to a skilled nursing facility (SNF), their care will be in the hands of a team of specialists. It’s a good idea to understand the players’ roles so you know whom to call upon for what.

Depression is common in older adults. It’s long been known that brisk exercise can help reduce depression. But it turns out that exercise doesn’t have to be vigorous to make a difference. Even mild exercise can be effective.

No one likes to dwell on the possibility of disaster. But we all need to prepare for one, just in case. Help your relatives gear up for safety. Whether you live across town or across the nation, the action items are the same.

If your loved one has balance problems, the culprit may be in the medicine. Many common medicines have side effects that can impair balance and lead to a fall. Over 40% of persons age 65 and older take five medications or more. This increases the chance that at least one of the drugs has side effects of dizziness, blurry vision, drowsiness, or muscle weakness.

Has your parent remarried? If so, you may be sharing the caregiving with a person you don’t know very well. Biological families often encounter tensions when it comes to eldercare. Add a stepparent and the challenges can grow exponentially.
Medicare pays for many screening exams, and even counseling sessions, to help nip common illnesses in the bud. Screening tests are designed to identify problems before symptoms emerge. They are usually for people who are considered to be “at risk” for getting a specific disease. Here are some of the most common noncancer preventive services that Medicare covers. Ask the doctor if your loved one should be tested.

Good communication requires both speaking and listening. Oddly enough, if you make a specific effort to listen, it can open doors. Once “heard,” the other person may be more willing to hear your point of view. Deep listening is more difficult than it sounds. It’s not passive. It requires concentration. It also takes humility and empathy.

For a teen, a relative’s dementia can turn a close relationship into one that’s now awkward, confusing, and embarrassing. And creates feelings of guilt.

After you have scoured the Internet to help your relative find a potential new doctor—someone on their plan and with no obvious red flags—it’s time to get more specific. The doctor’s website may provide some descriptive information, but most likely, you’ll want a conversation.

For most family caregivers, frustration and guilt are common, as is anxiety and resentment. These feelings are normal and reasonable under the circumstances. It’s not realistic to eliminate negative emotions. Caring for an ailing family member IS emotionally taxing, especially in the case of memory loss. But sometimes the negativity can feed on itself.

Even pre-COVID, many 90-year-olds adamantly refused to go to a senior center, saying they didn’t want to be around “all those old people.” (!) Does this sound like your loved one? Admittedly, the senior centers of the past tended to focus on bingo and crafts. These activities are of limited interest to the newest generation of older adults. Happily, senior centers have been updating. Bingo and crafts are still there. But the upswing in technology use during COVID catapulted many centers into the 21st century

With summer’s warm weather, be on the lookout for dehydration in your loved one. The signs include confusion, fatigue, weakness, and sleepiness. Some people become dizzy and their balance is thrown off. Dry mouth, headaches, and muscle cramps are other symptoms of dehydration.

If the person you care for has dementia—memory or thinking problems from a condition such as Alzheimer’s, a stroke, or Parkinson’s—unpaid bills or a messy checkbook may have been your first sign that something was amiss. Certainly, in the later stages of dementia, your loved one won’t be able to manage their finances. But what about the in-between?

Elderly parents are living longer. Children are often dependent for more years than expected. Add to this the ongoing responsibilities to spouse/partner and jobs, and there is little wiggle room for the millions of family caregivers who find themselves squeezed in the middle as the “Sandwich Generation.”

Many older adults experience swollen legs and feet. For some, it’s because of sitting a lot and leading a sedentary lifestyle. For others, it’s the water retention side effect of a medication. And for others, the swelling—called “edema”—is a symptom of a chronic or even serious illness such as heart failure or liver or kidney disease.
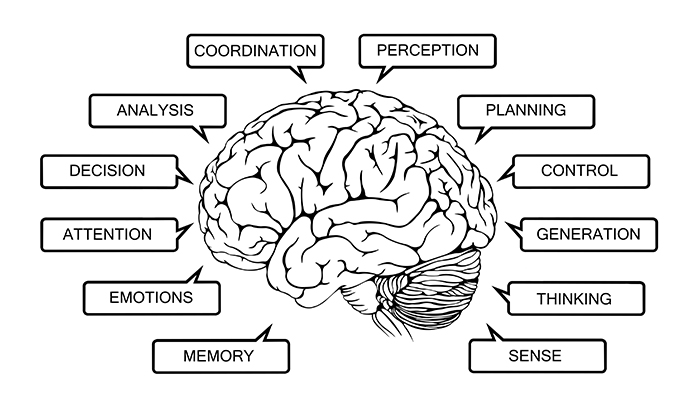
The brain is another organ to keep fit, and regular workouts are a good thing! Our brains enable many types of thinking: Problem solving, planning, attention, and memory. They manage our emotions and help us understand the emotions of others. Our brains also control movement (balance, speed, and coordination). And it’s where we process our spatial awareness—used for packing a suitcase or reading a map.
Much of the strain of caring for a loved one lies in the loss of a predictable routine, a sense of “normalcy.” Understanding the course of your loved one’s condition—the rhythm of how it unfolds—can empower you to respond more flexibly to its challenges.

Your loved one may be watching for phishing scams on email, but now there are scams carried out by short message service (aka, texting). “Smishing” scams rose 58% in 2021. Nationwide they cost victims over $10 billion. Seniors are a prime target, as three out of five now own smartphones. While convenient, smartphones present new opportunities for getting scammed. Time to alert your relative to smishing.

Children generally like to feel included. But they may not know how to relate to an ill family member with limited abilities. Here are some ideas for home-based activities with elementary-age children.

Has your loved one been diagnosed with cancer? The vast majority (67%) of people with cancer live for another five years or more. A cancer is considered “stable” or “controlled” when tumors shrink or at least temporarily stop growing. This is not the same as being cured—no tumors—but it does make cancer more of a manageable chronic disease, like diabetes or asthma.

Do you ever look at friends and find yourself mad or upset because they have free time? They don’t have a relative that needs help? You might even wish they had it harder, had some real challenge in their life. And then you feel guilty. If this sounds familiar, you are not alone. Envy is a natural human emotion.

A primary care provider (PCP) is charged with monitoring and treating a person’s whole body. Specialists abound and indeed are important. But we are more than the sum of our organs. Your relative’s PCP helps ensure that specialists are not doing things that counteract each other. If you are looking for a new PCP, there are several types of providers to consider.

Is low vision making it harder for your loved one to cook? If food preparation has been one of their pleasures, they are probably grieving not only the change in their eyesight, but also the loss of creating and serving delicious meals. Even if cooking has not been a passion, the ability to safely prepare food for oneself is critical for maintaining independence and self-esteem. Fortunately, there are ways to empower your relative with simple strategies and inexpensive tools. Here are some techniques that augment and use all the senses. They also protect safety.

We’re breathing all the time. But when it comes to stress relief, not all breathing is equal. Our bodies are built to handle periodic crises. When we sense danger, our bodies release “stress hormones” that enable us to respond powerfully and fast. When the crisis is over, those hormones are no longer released. The body returns to relaxed, “normal” mode. But chronic stress is damaging. When we’re stressed every day, the “fight-or-flight” hormones keep running. Not a lot, but enough to upset the body’s balance and undermine physical health and mood. The body is distracted from its routine tasks of repair and maintenance. This can result in significant consequences.
If the person you care for has dementia, you may have noticed their withdrawal from conversations, movies, even from reading books or the newspaper. Anything with an involved plot line is now too difficult for them to follow. Poetry, on the other hand, involves rhythm and images, which can stimulate memories of experiences, emotions, smells, tastes, and other sensations. All quite accessible by persons with dementia. Plus, many older adults went to school when poetry was an active part of the curriculum. Exploring fun poetry together may tap into positive memories from the past.

Those who donate organs, eyes, or tissue leave a tremendous legacy, often the gift of life itself: Allowing someone a steady heartbeat. Or the vision to see a grandchild. Or healthy skin to cover a burn or cancer site. National Healthcare Decisions Day (April 16) is when everyone is encouraged to create or update their advance directive. These end-of-life documents include a section for letting family members and healthcare providers know whether you choose to be an organ donor.

Combining households has many benefits: Less hassle running back and forth between two residences, less worry about Dad eating well and remembering his meds, more family social time for him, cost savings on rent and utilities, etc. But if things do not work out, disentangling could cause hurt feelings and damage your relationship. Consider these questions before you move in together.

Families spend three to five years caring for an aging relative. At first it may be light chores or small errands now and then. But over time, health challenges emerge and needs grow. In his book, My Mother, Your Mother, geriatrician Scott McCullough outlines eight “stations” in the journey of late life. For each one, he offers insights and tips to help you counter the modern system of “fast medicine” with personalized solutions he calls “slow medicine.”

People who go through chemotherapy for cancer often complain about “chemobrain.” If your loved one is under treatment and is having trouble with memory, thinking, and concentration, it is likely from the chemo drugs. The fuzzy thinking may not go away right when chemo stops. But it usually recedes over time.

Juggling multiple schedules, keeping other relatives informed, ensuring prescriptions are filled … these are but some of the many duties you may face as a family caregiver. In some instances, a simple spreadsheet can do the trick. But an app makes it easier to coordinate with others.

Anxiety and stress commonly accompany family caregiving. The ongoing pandemic and its stream of variants are only adding to that. Perhaps you could use a little “psychological first aid.” These are skills or techniques first responders are trained to teach or apply to distressed persons after urgent physical issues have been addressed.The goal of psychological first aid is to help people feel safe (physically and emotionally), calm, and hopeful. Connected to others. Sound good? Try these strategies on yourself.

Is Dad asking if he should sell the house now that Mom is gone? Or perhaps Aunt Mary is anxious about her stock investments. Even if you are good at managing your own money, helping a relative make financial decisions can bring a lot of pressure. Consider hiring a professional to advise you.

If a loved one in your life is undergoing chemotherapy for cancer, very likely they are dealing with the common side effects of nausea and vomiting. Not fun. Encourage them to follow these tips.

Care in a nursing home is expensive. For an extended stay, most people will need to pay quite a bit out of their own pocket. If there are no savings, Medicaid—the joint state-federal health insurance for low-income individuals—will step in.

Romance crime is on the rise. Over 25,000 people reported a sweetheart scam to the Federal Trade Commission (FTC) in 2019, a threefold increase since 2016. Individuals age 65 and older were the hardest hit, with a median loss of $9465 (across all ages, the median loss was $2500 per individual). If your loved one has been taken advantage of, they are not alone! Romance scams are the second most common crime reported to the FBI.

We all know the classic heart attack portrayed over and over again in movies and on TV: Someone writhing in sudden, severe chest pain.
But many heart attacks aren’t like that at all. Instead, they start slowly, typically with some mild, on/off pain or tightness in the chest. These signs are so much less dramatic than what people expect, they too often are ignored. The result, sadly, is often fatal when in fact a prompt response could have saved a loved one’s life.

In the last two weeks, as a loved one is nearing death, it is natural to want to be at their side. But then, what? Especially if you have never been in this situation before, you may feel uncertain—even awkward—about what to do. The ideal is to be a calm, reassuring, and loving presence focused on keeping your relative comfortable. Here are some tips.

The pandemic has brought on a wave of physician retirements. Perhaps one of your relative’s doctors has sent a letter announcing the close of their practice. Yikes!
When choosing a new physician, it’s worth the time to do some research. The right fit is critical to your loved one’s health and well-being.

If you are like most family caregivers, your social life has dropped in priority as you juggle your loved one’s needs. There just aren’t enough hours in the day to keep up all your friendships in addition to your family responsibilities.

Grief is the expected response to a loved one’s death. We expect to mourn, and we receive comfort from others. But in the context of a dementia, such as Alzheimer’s disease, the loss is not as clear cut. Your partner is “here but not here.” And you do not receive the same support or acknowledgment for the very real losses.

Time off from caregiving is precious. But after a break, many family caregivers find they don’t feel as refreshed as they hoped they would. Current research provides insights about how to get the most from a respite break.

If your loved one has health challenges, they may be feeling a loss of control. Add to that a terminal diagnosis and a sense of doom may prevail. But recognizing that life is coming to a close does not have to mean one waits glumly for the end. Following are some of the many ways hospice patients have chosen to take action and purposefully write their own “last chapter.” Perhaps one of these might appeal to your loved one:

Typically, it’s family members who fill in to perform the necessary tasks. But for many, perhaps including you, there are obstacles to helping on a regular basis. (Quitting your job to provide care is risky. Leaving work midcareer jeopardizes your retirement options and savings.)

Is your loved one having trouble hearing the television? Closed captioning isn’t helping enough? Check out these possible solutions.

It is usually obvious what a person with dementia is no longer able to do. But finding things your loved one CAN do may feel like a challenge, especially if memory loss is severe. Here are some tips:

For nonmedical support, check out community programs. Many are provided by nonprofit organizations. Others by faith communities. And still others by local government. Most offer discounts or a sliding-scale fee.

The holiday season is a festive time of year, but it may not feel much like a celebration for people grieving the loss of a loved one. Holidays are an especially tender time for missing those who are no longer with us.

Almost 3.5 million members of the military served in Vietnam between 1964 and 1975. Was your relative one of them? This group of veterans continues to face physical and mental health problems.

There are many undergarments designed to help with incontinence. They can’t prevent it, but they can help your loved one feel more comfortable with outings and retain their dignity despite the embarrassment of accidents.
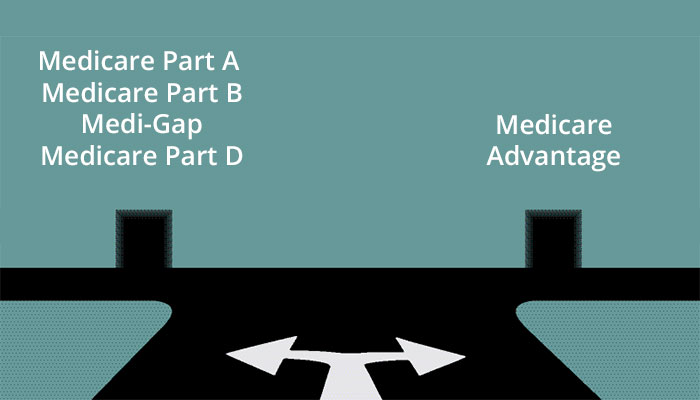
Once a year, Medicare offers the option to change plans. In 2021, the Open Enrollment period is October 15–December 7. Your loved one may be considering a switch to a “Medicare Advantage” plan. There are pros and cons.

If the person you care for has a life-threatening illness, you might think it’s only natural for them to feel down. Even hopeless from time to time.
But weeks of sadness are not a side effect one simply has to tolerate. It is not uncommon for someone with cancer or a similarly scary diagnosis to become depressed. But depression can and should be treated. Effective treatment makes for better quality of life. It can also improve other symptoms, such as pain and insomnia.

More than half of older adults take five or more medications per day. That’s “polypharmacy,” and can be dangerous. Taking too many medicines can cause problems such as dizziness, mental confusion, and heart failure. It can create an increased risk of falls, which often lead to the end of independent living. An estimated 10% to 30% of older adult hospitalizations are due to medication problems.

If the person you care for has Alzheimer’s disease or another type of dementia, you may find their sudden emotional swings more difficult than their forgetfulness. Among many things, the disease has taken away their inhibitions. They can become quite irrational. And they are more likely to make a scene in public than they ever would have before their dementia. Family members mention embarrassment as one of the most difficult aspects of caring for their relative.

One of the most challenging dilemmas when caring for an aging parent is balancing their preference for independence with your concern for their safety. If you have noticed lapses in cleanliness, meals, bill payment, or other areas, you may be worried that your loved one is not able to safely live alone. They may refuse assistance, however, not recognizing there is a problem.

What do a marathon runner and your aging parent have in common? Both could benefit from compression socks! By applying pressure to the legs, compression socks help the valves in the veins do their work—so blood is pushed back to the heart and doesn’t pool in the legs. Older adults with edema (swollen legs), varicose veins, or deep vein thrombosis find that compression socks ease discomfort and can even prevent problems.

It’s only natural for family caregivers to worry. Understandably, we spend a lot of time thinking about “what’s next.” But if you are in a pattern of persistent worry and are starting to feel the stress in your body too—perhaps headaches, loss of appetite, or trouble sleeping—you may be dealing with anxiety.
Medicare is health insurance provided by the federal government. It covers adults 65 and older, as well as persons with disabilities. In terms of home care, Medicare pays for visits only by medically trained staff. In that light, there are two programs: Home health and hospice.
When your family member is in pain, you are suffering, too. The “mirror neurons” in our brains are programmed to recognize pain in others. That’s good news in that it arouses compassion and spurs us to action. But it can be bad news, too. When you are highly attuned to a loved one’s pain, you are at higher risk of depression, burnout, and poor health yourself.
© 2002-2024, LiveWell Elder Care Management. Site created by Elder Pages Online, LLC.